The Invisible Epidemic: Autoimmune Disease
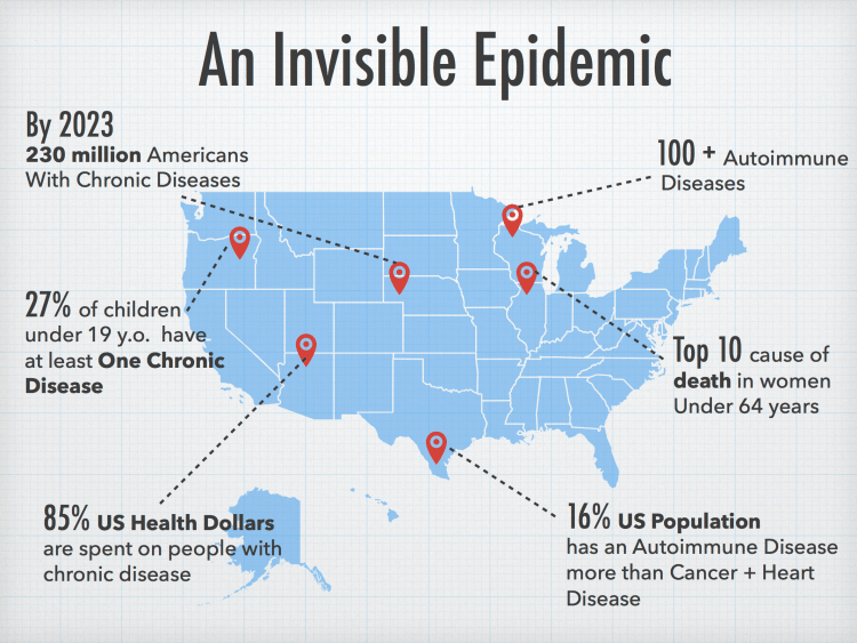
There are over known 100 autoimmune diseases costing the US over $100 billion annually, yet there are still many unknowns about autoimmunity, what causes it, and how it should be treated.
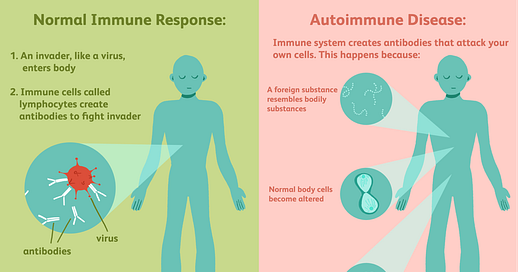
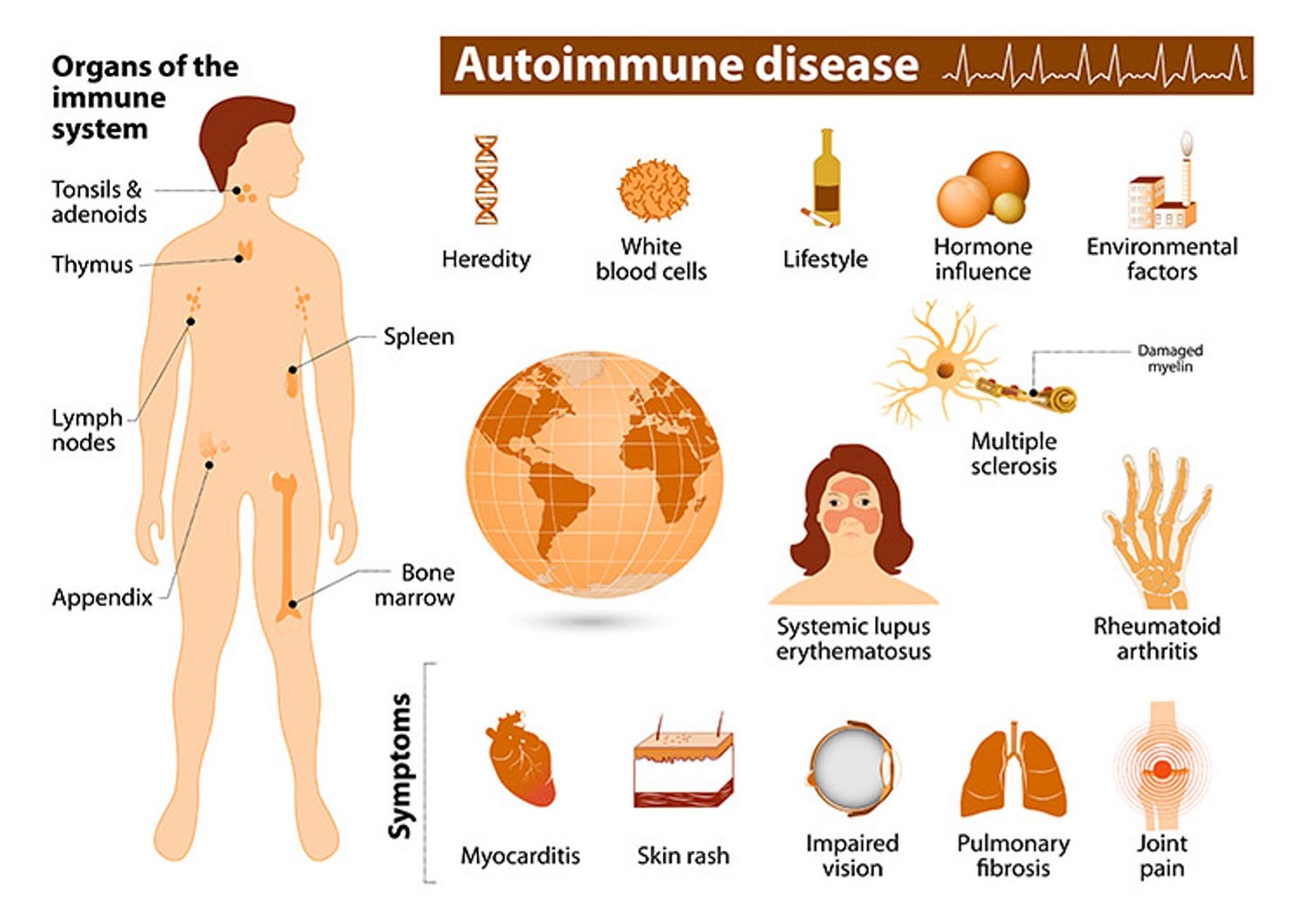
Autoimmune diseases occur when the immune system mistakenly attacks healthy cells, tissues, and organs in the body, leading to a wide arrange of symptoms and potential damage. They can affect any part of the body and weaken bodily functions to various extents and in rare cases can be life threatening. Autoimmune diseases in general cannot be cured, but with medication, lifestyle changes, and other treatment methods can be managed.
In recent years, autoimmune diseases have been top of mind for providers and patients with an increasing number of individuals diagnosed with some form of the disease. Research indicates that a specific type of autoantibody (an antibody produced by the immune system that is directed against one or more of the individual’s own proteins) called antinuclear antibodies increased almost 50% in the U.S. in a span of 30 years. Internationally, the incidence of autoimmune diseases is rising by approximately 3% to 9% annually, with significant increases noted in regions previously less affected, such as the Middle East and East Asia. Today there are over 100 known autoimmune diseases affecting 1 in 10 people with 13% of women and 7% of men worldwide impacted it. In the US alone it’s estimated up to 50 million people are affected, with 75% of this population being female making it one of the most prevalent disease categories.
The increase in autoimmune disease prevalence is thought to be influenced by several factors. A combination of genetic, environmental, and lifestyle factors are likely key contributors. Certain genes increase your susceptibility to autoimmune diseases, although genetics alone does not directly cause the diseases. There is a hypothesis that increased hygiene has contributed to the increase in autoimmune disorders due to the reduced exposure to pathogens, potentially leading our immune systems to attack itself versus foreign invaders. Another environmental factor that has been frequently discussed is our increased exposure to pollution and chemicals which are thought to trigger the immune system to start attacked the body’s own cells. Dietary changes are often cited as another potential contributor due to ultra-processed food and unnecessary additives in our diets. Psychological stress has also been shown to activate the immune system, potentially triggering autoimmune responses. Certain infections can also trigger autoimmune disease as well as changes in sleep patterns which contribute to immune dysregulation.
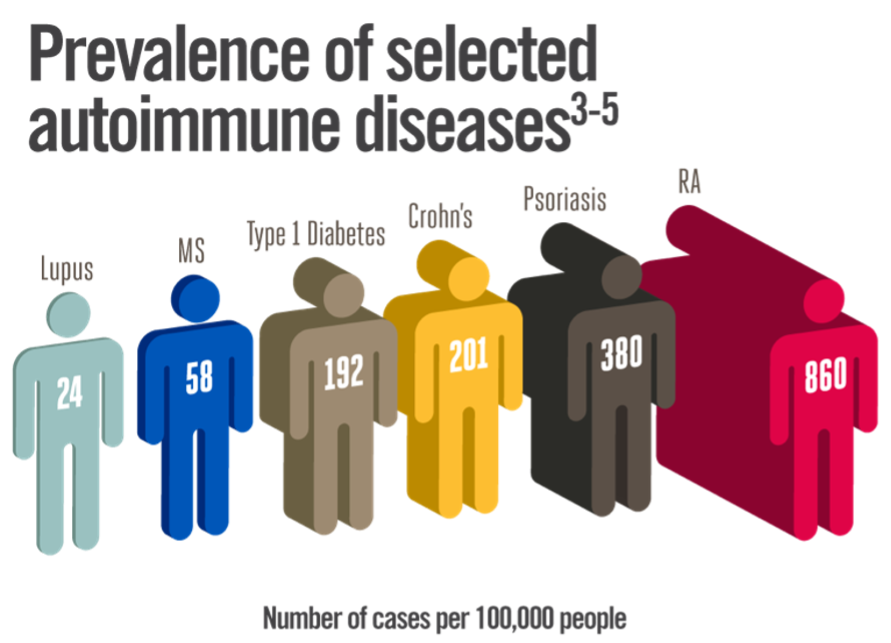
The most common autoimmune diseases are rheumatoid arthritis, lupus, type 1 diabetes, multiple sclerosis (MS), inflammatory bowel disease (IBD), psoriasis, Hashimoto’s, and Graves’ disease.
Rheumatoid Arthritis affects the joints, causing pain, swelling, and potential loss of function.
Lupus can affect the skin, joints, kidneys, brain, and other organs.
Type 1 Diabetes targets the pancreas, impairing its ability to produce insulin.
MS affects the central nervous system, leading to various neurological symptoms.
IBD includes Crohn’s. disease and ulcerative colitis, affecting the gastrointestinal tract.
Psoriasis affects the skin and can also lead to joint issues.
Hashimoto’s leads to hypothyroidism due to thyroid gland inflammation.
Grave’s Disease results in hyperthyroidism, where the thyroid gland is overactive.
The main challenge of autoimmune disease is the fact that many often present with non-specific symptoms that can vary widely between individuals, often impairing our ability to diagnose and treat the diseases. Some of the ways in which we currently diagnose autoimmune disease are nonspecific and a bit antiquated leading to an average diagnosis length of 4.5 years. There are symptom assessments and a plethora of blood tests that scan for antinuclear antibodies, autoantibodies, complete blood count, c-reactive proteins, and erythrocyte sedimentation rate. Symptoms often flare on and off making this extremely difficult for patients and often leading them to self-diagnose given historical dismissiveness of doctors.
As far as treatment goes, the protocol is just as bleak with no known cures and an array of often unsuccessful symptom management tools. Patients can be put on immunosuppressive drugs, such as corticosteroids and non-steroid agents, go through physical therapy regimens and even dietary changes and supplementation plans, while being regularly monitored to adjust and adapt treatment plans. Autoimmune diseases are particularly hard to treat due to their complex nature and the body’s immune system involvement.
They can affect almost any part of the body which makes it difficult to predict how the disease will progress and respond to treatment. They vary wildly in symptoms and disease expression, meaning two individuals with the same disease can present very differently. On top of these difficulties, many of the current treatments for these diseases can have significant side effects, so managing these while trying to suppress the autoimmune system response is a delicate balance. Diagnostics have fallen flat when trying to determine appropriate treatment and we are still a way away from a research perspective in understanding these diseases posing a challenge to disease-specific treatment development. Most current therapies are broadly acting and non-disease specific which can lead to unwanted immunosuppression and associated complications for patients.
One topic regarding autoimmune care that has recently become popular is the impact that lifestyle change can have on these diseases. Researchers and health professionals have found that lifestyle modifications play a significant role in managing and potentially alleviating symptoms of autoimmune disease. These changes can reduce inflammation, enhance gut health, and improve overall well-being. There are 5 main categories of lifestyle modifications that have been shown to improve symptoms of autoimmune disease: dietary changes, exercise, stress management, sleep, and avoidance of environmental toxins.
Dietary changes can alleviate many of the symptoms associated with autoimmune disorders, specifically instances of IBD. Many initial treatment protocols for gut related autoimmune disease call for elimination diets to identify if certain foods are responsible for adverse symptoms. Examples include low FODMAP, paleo, or specific carbohydrate diets. Anti-inflammatory diets that include foods high in omega-3 fatty acids and antioxidants, while removing inflammatory foods like gluten and diary, can significantly reduce symptoms. Some health professionals even suggest incorporating fermented foods and those rich in probiotics to help improve gut health.
Outside of diet, exercise, stress management and sleep are crucial components of dealing with autoimmune disease. Exercise is an essential part of a healthy lifestyle, beyond physical benefits there are so many things exercise can help with (see my recent newsletter on weight lifting for more information). Regular physical activity can help improve circulation, reduce inflammation and pain, and enhance overall physical and mental health. Stress management is also important when dealing with autoimmune disease because stress often exacerbates symptoms. Techniques such as meditation, yoga, and deep-breathing exercises can reduce stress. Sleep is a key element of our health and getting adequate sleep can drastically improve symptoms associated with autoimmune diseases. Sleep is essential for recovery and maintenance of immune system balance and disruptions in sleep can lead to increased inflammation and adversely affect autoimmune disease outcomes.
Another huge component of a healthy immune system is our environment. More recently, there has been a heightened focus on removal of toxins from our everyday lives due to many studies that have shown negative effects of toxins from household items on our immune system. Consumer brands like Branch Basics for household cleaners, Ilia for makeup, Caraway for cookware, and more are more popular than ever as consumers have become more educated on how environmental toxins commonly found in everyday products can affect our overall health and immune systems. Beyond household toxins, other environmental pollutants such as silica, mercury, pristane, dioxin, are released through combustion plants, mining, fishing in polluted waters, etc. and cause harm our immune system when inhaled, consumed, or upon skin contact. Minimizing exposure to these types of toxins by using natural products can decrease the body’s toxic burden and help manage autoimmune responses.
Lifestyle changes are a vital component of integrative medicine approaches for treating autoimmune diseases, often used in conjunction with traditional medical treatments such as medication. Many have claimed that lifestyle interventions have seemingly “cured” them of their autoimmune diseases, but ultimately the effectiveness of these interventions can vary based on genetic predispositions, disease severity, and individual patient responses.
There are a number of companies emerging across the spectrum of healthcare that are targeting the autoimmune disease market. WellTheory is a digital solution targeting individuals with autoimmune immune disease and offers evidence-based nutrition and lifestyle coaching to reduce symptoms and help patients overcome the struggles of living with autoimmune diseases. Paloma Health is another digital platform in the space, specifically servicing the millions of people who have been diagnosed with Hashimoto’s or hypothyroidism by matching patients with thyroid doctors that help them manage their symptoms and get access to medication. Veracity is an online marketplace and maker of diagnostic tests as well as skin, gut, and vitamin supplements that aim to naturally heal hormone imbalances and help individuals manage symptoms often associate with autoimmune disease. Cour Pharmaceuticals’ nanoparticles reprogram the immune system to stop inflammation behind autoimmune disease.
These are just a few of the companies working to improve outcomes from autoimmune disorders, but there is still a long way to go to make progress in the space. It is crucial that we continue to fund both companies building in the space, but also research and training of health care professionals so that we can better understand the root causes and develop potential treatments and prevention strategies for these diseases. It is also important that we, as consumers, are educated on the effects of lifestyle changes and environmental factors on our immune system and how we can optimize our health and hopefully, avoid autoimmune disease altogether.